

Journal of Multidisciplinary Dental Research
DOI: 10.38138/JMDR/v6i1.5
Volume: 6, Issue: 1, Pages: 27–32
Case Report
Nezar Watted1,2,*, Mohamad Abu-Hussein3 , Ali Watted4 , Borbély Péter5
1Klinik und Polikliniken für Zahn- Mund- und Kieferkrankheiten der Julius- Maximilians-Universität Würzburg /Deutschland, University of Debrecen/ Hungary
2Faculty of Dentistry of the University of Sevilla/Spain, Arab American University/ Jenin
3Department of Pediatric Dentistry, University of Athens,Greece
4Zentrum Zahn-, Mund- und Kieferkrankeiten, Klinik für Mund- Kiefer- und Gesichtschirurgie der Universität Hannover,Deutschland
5Department of Orthodontics, University of Debrecen, Hungary
* Corresponding author
Nezar Watted
Email: nezar.watted@gmx.net
Received Date:27 June 2020, Accepted Date:08 July 2020, Published Date:31 August 2020
Recently, a continuing trend cannot be overlooked: the number of orthodontically treated adult patients, with a particular interest in the correction of aesthetic imbalances, is increasing continuously. Because the mouth and teeth play a significant role in the attractiveness of the human face and the teeth are viewed as a prominent feature of personal identity, the correction of dentofacial anomalies must be realized with the appropriate emphasis on the objective goal-setting in orthodontics. Adult treatment itself confronts the orthodontist with interdisciplinary questions that, for example, concern orthodontic tooth movements in periodontally damaged section of the jaw.The high success rates of newer periodontal treatment techniques - such as guided tissue or bone regeneration— raised the questions of how these could reasonably be employed in combined periodontal- orthodontic therapy.
Keywords: Guided tissue regeneration (GTR); pathologic tooth migration; advanced periodontitis
Periodontal pathology has a multifactorial etiology. If left untreated it can lead to severe damage to the supporting structures and affect the treatment outcomes of different all specialties of dental practice.
The primary objective of periodontal therapy is to restore and maintain the health and integrity of attachment apparatus of teeth. Orthodontic therapy is aimed not only to improve facial esthetics and function but also to address to the health of supporting structures 1. Hence, an interdisciplinary treatment approach is the key to successful diagnosis & treatment planning. The interrelationship between orthodontics and periodontics often resembles symbiosis. In many cases, periodontal health is improved by orthodontic tooth movement and orthodontic tooth movement is often facilitated by periodontal therapy. Both the short and long term successful outcomes of orthodontic treatment are influenced by the patient’s periodontal status before, during and after active orthodontic therapy including post treatment maintenance by the patient 2, 3 . Orthodontic bodily movement into plaque induced infra bony defects can be successfully performed, provided that the periodontal lesion is eliminated before tooth movement is began, and excellent oral hygiene is maintained. Orthodontic treatment in patients with compromised periodontium differs considerably from that performed in subjects with healthy periodontium. One should be aware of the biomechanics and the importance of the treatment sequence. The key elements are listed as follows: (1) Formulation of a tailor-made comprehensive treatment plan consisting of hygienic, corrective and maintenance phases; (2) Orthodontic treatment undertaken within clinically healthy periodontium; (3)Use of lighter force with greater moment and force ratios; (4) Establishment of a stable anchor; (5) Close monitoring of treatment progress; (6) Regular periodontal care during active orthodontic tooth movement; (7) Establishing appropriate retention after orthodontic treatment; and (8) Long term periodontal maintenance care. 1, 3, 4, 5 It has been shown that it is possible to regain bone attachment levels lost to periodontitis or trauma. Researchers suggested that the healing of the periodontium was determined by the cell type that repopulated the wound surface. This concept of selective cell population influenced Nyman et al. 6 to use occlusive barriers in the periodontal healing studies that formed the basis for a technique later known as guided tissue regeneration –GTR-Figure 1, Figure 2.


Essentially, GTR is used in different types of periodontal defects (1-, 2-, and 3-walled lesions) to attempt to regenerate lost periodontal structures through differential tissue response. This is accomplished with a barrier membrane to prevent the cells from the gingival connective tissue and the epithelium (fast proliferative capacity) from colonizing the decontaminated root surface in the belief that these interfere with regeneration. This allows for the proliferation (slow turnover) of cells derived from the residual periodontal ligament (PDL) and from bone marrow spaces to promote periodontal regeneration with subsequent matrix deposition and bone mineralization. 1, 5, 6, 7 Regeneration is a very complex phenomenon that depends on a coordinated response from several cell types that produce a wide range of extracellular matrix proteins.7, 8 The impact of GTR to patients before, during, or after orthodontic treatment has been occasionally reported in the literature. Similarly, there is little information on the effects of osseous defects such as dehiscences, fenestrations, and localized ridge deformities in the orthodontic treatment plan. To repair these localized bony ridge defects, a similar technique to GTR has been called guided bone regeneration (GBR), because its main purpose is not to induce new tissue around a tooth but to regain an adequate bony alveolar ridge. 4, 7, 9, 10 This article describes the orthodontic treatment of an adult who underwent GBR and decalcified freeze-dried bone allografts to repair an osseous defect caused by the extraction of a premolar before orthodontic tooth movement. This report and similar reports should reinforce the concepts of regenerative procedures as possible complements to specific orthodontic treatment plans.
Case report
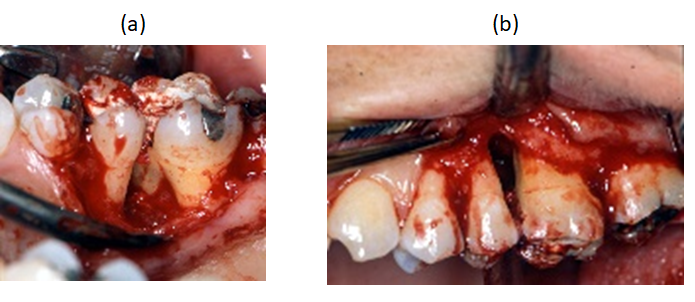
A 38-year-old female patient presented to our practice for orthodontic treatment. The intraoral photos showed class I occlusion on the right and left. The top view photos showed the dental malpositioning in both arches and crowding in both fronts. According to the patient, none of the lower jaw front teeth had been extracted, which confirmed agenesia of a front tooth (Figure 3 a-d). At clinical examination and when recording periodontal status, a pronounced pocket depth (12mm) of tooth 26 was determined mesially, buccally and palatally ( Figure 3 e). There was first degree loosening and zero for the adjacent teeth. The gingival appeared unphysiological (red and oedematous). These findings were confirmed radiologically with demonstration of massive bone loss, which can be seen only mesially, representing a localized periodontitis marginalis profunda (Figure 4 ). After motivation and detailed oral hygiene instruction, the first treatment phase (initial therapy) began. In the root planning phase, a mouth rinse (Dentaleen/Jatt/Israel)) and antibiotics were prescribed. After the first treatment phase and thanks to the patient’s excellent cooperation, the papillae bleeding index (PBI) and approximal plaque index (API) were reduced to almost zero. Periodontal surgery followed several weeks later. During the surgical procedure, a large bone defect was revealed that affected the entire root length of the molar (Figure 5 a, b). Root planing and removal of infected soft tissue was then carried out. The removal of the entire infected hard and soft tissue is a fundamental requirement for the success of guided tissue or bone regeneration. To support the procedure, ultrasound was implemented for the subgingival scaling. Guided tissue regeneration (GTR) in combination with a bone implant was used for regenerating the periodontal defect. A demineralised freeze dried bone product (particle size 1000–2000mm, Dexabon, CardioPhil) was used. An absorbable membrane was used as a barrier between the bone-filled defect and the gingival epithelium (Hypro-Sorb F, Resorbable Bilayer Collagen Membrane, CardioPhil). Careful clinical examination with review of the periodontal status was done five months postoperatively. An attachment gain was diagnosed at the preoperatively deepest point and there was regeneration of the alveolar bone buccolingually and vertically.
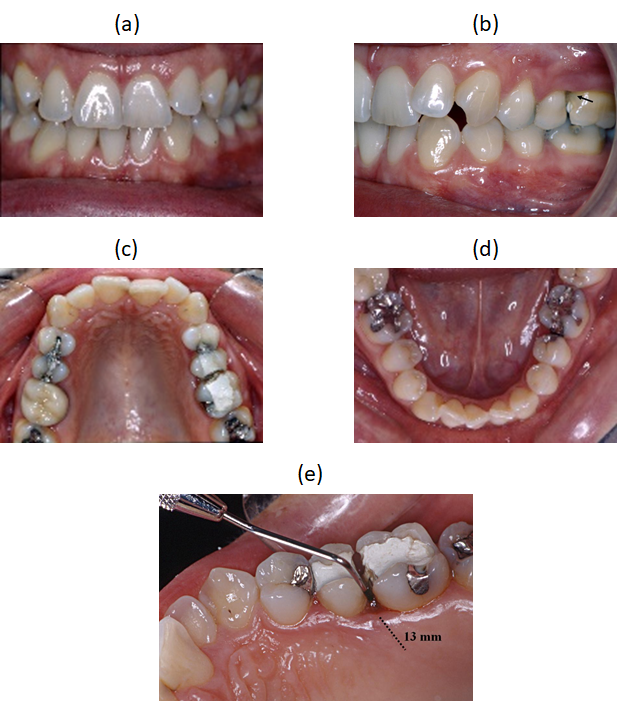

These positive results were the prerequisite for orthodontic therapy with the goal to resolve the frontal crowding. A prosthetic tooth replacement of the absent front tooth in the lower jaw was not planned. It was planned to distribute the resulting gap over the entire frontal region, so that tooth expansion with composite could be done. Both arches were bonded with a multibanded orthodontic appliance. The upper front teeth were stripped (enamel reduction), in order to create a harmonious tooth shape in the upper front and to prevent excessive protrusion of the front teeth (Figure 6). The orthodontic treatment was carried out gradually and with low controlled forces. Additionally, the patient was enrolled in a monthly recall program. Upon conclusion of the orthodontic treatment, expansion of the lower front teeth and formal correction of both upper cuspids was done (Figs. 7 a, b). A retainer was bonded in both fronts. The clinical images show a gap-free front segment (Figs. 8 a-c). Figure 9 shows the bone conditions in the regenerated region into which tooth 26 was moved.

Fig. 6: Enamel reduction: stripping of the upper front
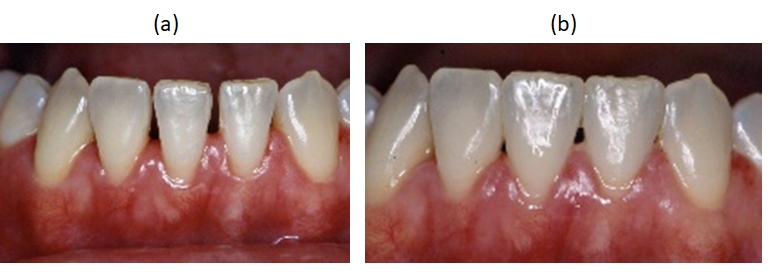
Fig. 7: a-b The gaps in the lower front were eliminated through tooth expansion with composite mass
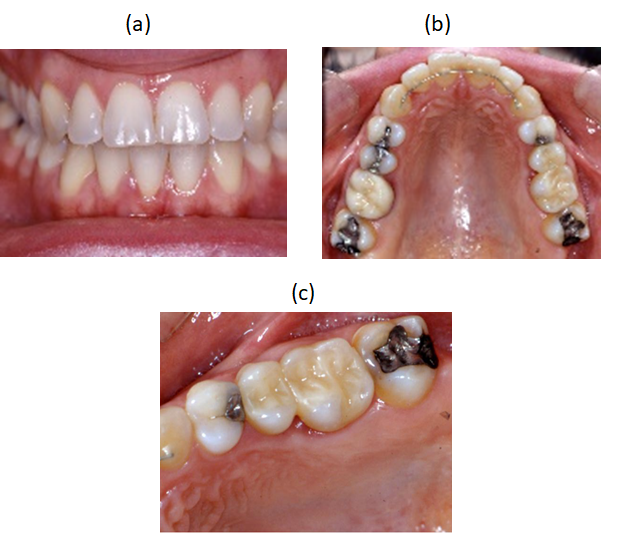
Fig. 8: a-c Situation at completion of the entire treatment (orthodontics, periodontal and conservative)
Fig. 9: Situation after completion of orthodontic treatment. The augmentation was done in the context of the periodontal treatment and prior to orthodontic treatment
Orthodontic treatment is based on the principle that if prolonged, controlled force is applied to a tooth, tooth movement will occur as the bone around the tooth remodels. Bone is selectively removed from some areas and deposited in others 8, 11. In essence the tooth moves through the bone, carrying its attachment apparatus with it, as the socket of the tooth migrates. With the success of the fixed multi banded appliance in the recent decades, orthodontic treatment in adults has continuously grown. But the assessment of periodontal status and maintenance of its health is of paramount importance for the success of this treatment 12, 13, 14. A treatment plan with an interdisciplinary mindset can transform an unaesthetic dentition with compromised periodontal health into a healthy an attractive solution for the patient 2, 15. Adult orthodontics has been the subject of numerous discussions. Significant developments have taken place since the beginning of the century when orthodontic treatment was considered to be of very limited value after cessation of growth. Many adult patients suffer from periodontal disease which indirectly has contributed to the development or augmentation of the malocclusion being treated. With a decreasing level of periodontal attachment, the center of resistance is displaced apically. This implies that forces that, in the case of normal bone level are part of an equilibrium, in the case of bone loss will result in spontaneous migration and in spacing and increased overjet and overbite. Inflammation of the periodontal ligament can increase periodontal tension and lead to extrusion of teeth where this is not prevented by occlusal forces. 2, 4, 7, 12, 13 Rateitschak classified patients with periodontal disease who need orthodontic treatment in three categories 8.
Malposition that has always existed since completion of tooth eruption.
Tooth migration that has arisen through oral parafunctions
Tooth migrations caused by degenerative or dystrophic periodontal disease.
Many patients do not end their treatment with an ideal occlusion. Marginal bone loss may have resulted in apical displacement of the center of resistance to a degree that normal function is not compatible with equilibrium between the forces and resistance. Therefore, the teeth must be splinted to prevent spontaneous migrations 8. The key element in the orthodontic management of adult patients with periodontal diseases is to eliminate or reduce plaque accumulation and gingival inflammation. The combination of inflammation, orthodontic forces and occlusal trauma leads to more rapid destruction than that would occur with inflammation alone. In a study done by Artun and Urbye (1988) on 24 patients with advanced loss of marginal bone and pathological tooth migration, who received active appliance therapy for an average of seven months following periodontal therapy, the post-operative radiographs showed little or no loss of bone support 8, 11, 14.
Anchorage and retention play an important role in orthodontic treatment. Biological retention includes the necessary measures needed to maintain an optimal periodontal support. This is ensured through optimal oral hygiene, regular periodontal control and an occlusion that transfers occlusal forces in a vector passing as close to the center of resistance of the tooth as possible in order to avoid occlusal trauma. Similarly all existing teeth should be included in the occlusion because lack of force to a tooth will result in dystrophy of the surrounding bone and weakening of the periodontal ligament 1, 8, 11, 15. It is crucial to inform the patient that the dental status at the end of treatment requires constant periodontal and functional maintenance. The patient should be aware that the treatment result is a biological status that is under constant changes and he/she is largely responsible for its maintenance. The direct effect of orthodontic treatment on the periodontal status is controversial 1, 3, 9, 16.
It has been shown that orthodontic treatment may favour the destructive effect of the plaque associated inflammatory lesion in a thin gingival unit which is already susceptible to breakdown. In thicker layer of soft tissues, orthodontic tooth movement did not accelerate the breakdown. Studies done by Melsen 1986, on adult orthodontic patients say that the periodontal status be brought under control before orthodontic treatment is initiated 10.
Bollen et al. in the year 2008 conducted 2 systematic reviews on the orthodontic and periodontic interaction. In the first review they found a positive correlation between the presence of malocclusion and the incidence of periodontal disease. The second review addressed the effect of orthodontic treatment of periodontal health 17, 16. Bollen conducted another systematic review which concluded that orthodontic treatment was associated with 0.03mm gingival recession, 0.13mm alveolar bone loss and 0.23mm of pocket depth 17, 16.
Clinical situations where orthodontics should be avoided:
Uncontrolled infection and inflammation
Lack of retention for stabilization of teeth in their new position.
Inadequate space into which teeth can be moved
Movement of teeth against occlusal opposition or into occlusal trauma
Movement of teeth in conditions where periodontal health, function or esthetics will not improve
Movement of teeth against inadequate anchorage
Movement of teeth into unfavourable environment
Lack of patient motivation and co-operation
Tooth movement in patients with systemic problems that cannot be treated or are difficult to control 12.
Periodontal regeneration can be described as de novo cementogenesis, osteogenesis, and regeneration of newly formed fibers inserting into both newly formed cementum and alveolar bone. According to the American Academy of Periodontology, regeneration is defined as the “reproduction or reconstitution of a lost or injured part 16, 18, 19. However, if the healing outcome of periodontal treatment is via repair mechanisms, and not regenerative ones as described above, the newly formed tissue does not restore the architecture of the lost tissue. Even though new cementum and a PDL might be obtainable with techniques such as GTR, new bone growth might not always occur. Bowers et al. have shown that bone allografts appear to produce regeneration histologically. These procedures are especially indicated for vertical bony defects. Biomodification of root surfaces has also been suggested as an adjunct in regenerative PDL techniques. Citric acid and tetracycline have been used to promote greater connective tissue attachment both in vitro and in vivo 19, 20. The mode of action of bone grafts with Gore-Tex or other types of membrane can be classified as osteoconductive. Osteoconduction occurs when a physical matrix or scaffolding is present, allowing for bone apposition, if this takes place over existing bone or differentiated mesenchymal cells. The result described here was made possible by the formation of a matrix (in which new bone grew) through the placement of. Based decalcified freeze-dried bone allografts on our results, it can be assumed that osteoconduction or possibly osteoinduction took place, ultimately resulting in osteogenesis. By constrast, only autogeneous bone grafts (typically harvested from the iliac crest or another intraoral site) have the necessary combination of inductive bioactive molecules responsible for new bone formation. Such de novo induction and morphogenesis of periodontal tissue can enhance the use of gene-related products with inductive and morphogenetic properties that have been termed bone morphogenetic proteins (BMPs) 15, 18, 19. BMPs, particularly rhBMP-2, can bring about bone induction by stimulating the pluripotential or precursor cells of the host wall or from the cancellous portion of any bone graft placed in conjunction with the inductor material. Once undifferentiated cells are stimulated into the endochondral pathway, they will regulate osteogenic cells that are already committed to osteogenesis. The combination of BMPs and decalcified freeze-dried bone allografts helps expose the underlying bone collagen and BMP type growth factors from the decalcified freeze-dried bone allografts, enhancing the purported osteoinductive ability of these preparations 8, 18 . This is important because it is believed that alone c decalcified freeze-dried bone allografts cannot induce new bone formation at sites not normally considered capable of de novo osteoactivity. It has also been shown that, in the presence of BMPs, bone formation occurs heterotopically. Although it is still difficult to speculate into the clinical applications of these proteins, their induction of tissue morphogenesis through cementogenesis and periodontal regeneration is an essential ingredient of periodontal regeneration 8, 18, 19. However, in our case, one might speculate that, at 2 months after grafting, the regenerate was encouraged via the distal movement of the canine to proliferate coronally or bucally. One can also only conjecture whether there might have been a much less favorable osteogenic response if the distal movement of the canine had begun into the healing extraction site with an accompanying alveolar defect from the traumatic removal of the first premolar without having first performed the GBR procedure 8, 12, 16, 18, 19, 20.
This case report shows the advantage of using regenerative therapy to regain alveolar bone in a traumatic extraction site to prevent additional attachment loss due to orthodontic movement into the defect. We speculate that defects in similar cases (ie, with long-term extraction of permanent teeth in the mandibular arch resulting in atrophy of the alveolar ridge buccolingual dimension) can be treated similarly. However, in any of these circumstances, type and magnitude of the lesion as well as clinical variability will highly influence the success rate of regenerative procedures. Thus, it is important to report both clinical successes and failures to determine which defects respond most favorably to regeneration combined with orthodontic therapy. We hope that similar case reports will continue to define the interrelationship between orthodontic treatment and GTR principles.
© 2020 Published by International Dental Educationists’ Association (IDEA). This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
Subscribe now for latest articles, news.