Journal of Multidisciplinary Dental Research
Volume: 4, Issue: 2, Pages: 31-36
Original Article
Putu Toya Prastana Anggara1, Pricillia Priska Sianita2
1Student, profession programme, Faculty of Dentistry, Prof.DR.Moestopo University
2Lecturer, Faculty of Dentistry, Prof. DR.Moestopo University
Corresponding
Pricillia Priksa Sianita
Lecturer, Faculty of Dentistry, Prof. DR.Moestopo University
e-mail: [email protected]
Received Date:01 October 2018, Accepted Date:10 October 2018, Published Date:23 October 2018
Background: The prevalence of malocclusion in Indonesia is still very high, about 80 % of the population and therefore a major dental and oral health issue to be reckoned with. Population in Indonesia which is dominated by Deuteromalay sub-race has conveks profile characteristic with Angle class II division 1 malocclusion. According to Angle, class II division 1 malocclusion is almost always followed and aggravated or eveb associated with mouth-breathing habit as a result of blockage of the upper respiratory tract.
Objective:This study aims to detrmine the condition of respiratory tract in Angle malocclusion of class II division 1 from Deuteromalay sub-racial patients in Faculty of Dentistry, University Prof.DR.Moestopo.
Materials and methods: A total of 32 Deuteromalay sub-racial patients who met the inclusion criteria such as among others never undergone orthodontic treatment, were willing to be made lateral cephalometric radiographs and had Angle malocclusion of class II division 1 was collected by purposive sampling method. The radiogrph of this study was then traced for further analysis of the upper and lower pharynx according to the McNamara method.
Results: In the upper pharyngeal analysis, it was observed that all subjects had obstruction, while the results of lower pharyngeal analysis showed that twenty subjects had normal conditions and only 12 subjects showed obstruction.
Conclusion: all subjects of this study experienced upper respiratory tract obstruction. This fact indicates that the dentist has the ability to detect the presence or absence of obstruction or disturbances in the upper respiratory tract that may affect the occurance of class II division 1 malocclusion. If detection of the condition of respiratory tract is done early then the precautions or orthodontic interception can be done with the results which is more beneficial for the aesthetics of facial apprearance and patient profile.
Key words: class II division 1 malocclusion, upper pharyngeal analysis, lower pharyngeal analysis
One of the serious dental and oral health problems in Indonesia is the high prevalence of malocclusion, which reaches 80% of the population. This shows the importance of striving 1for a step / action both prevention and treatment. In this connection, malocclusion is understood as a condition where there is a mismatch of dental relationships or deviant jaw relations from normal.1 Malocclusion is also a deviation from growth and development, especially muscle and jawbone in childhood and adolescence and may be related to the bad habits they have at an early age.2 In 1907, Angle suggested that class II division 1 malocclusion was always followed or associated with the habit of breathing through the mouth which may be caused by blockage of the upper respiratory tract.3 Class II division 1 malocclusion is a malrelation characterized by increased overjet and overbite.4 The increase in overjet in this situation, especially is apparent so that it affects the face profile which generally will look convex. In this case, the upper anterior teeth often show a protrusive position while the relation of the maxillary first molar also shows class II relations or distal step or disto-occlusion. Deviation of growth and development in the jawbone will have an impact on the skeletal pattern of class II which also plays a role in producing a convex facial profile.5
Respiratory disorders can cause craniofacial malformations, jaw malocclusion and deformation. The normal and well-developed respiratory tract allows breathing through the nose normally with the mouth closed. Breathing through the nose is very important to get good health. The good benefits of breathing through the nose begin within a few hours after birth with the detection of nitrogen oxide gas for the first time.
This nitrogen oxide is produced in the nasal sinus and then secreted to the respiratory tract and inhaled through the nose. Nitrogen oxide can prevent bacterial growth and in the lungs, nitrogen oxide can increase the ability to absorb oxygen, as well as being a vasodilator and a powerful brain transmitter. Nitrogen oxide increases the transportation of oxygen throughout the body so it is very important for all organs of the body.3,6
Upper respiratory tract obstruction in children can cause sleep disturbances and sleep apnea which in the long term can result in, among others, failure in academic performance, behavioral disorders such as Attention Deficit Hyperactivity Disorder (ADHD), obstruction of physical development that affects body weight and height.3,6Therefore, if the obstruction of breathing is detected early and treated properly, the accompanying negative effects can also be avoided.
Moving on from this thought, this study was conducted with the aim of evaluating the condition of the respiratory tract of patients with Class II division 1 of Angle malocclusion who came to the dental health clinic at the Faculty of Dentistry, Prof.Dr.Moestopo University.
MATERIALS AND METHODS
This research was conducted in July 2017 at the dental clinic of faculty of dentistry Prof.DR.Moestopo University in Jakarta. The subjects in this study were selected using a purposive sampling method with several inclusion criteria as follows: patients had Angle class II division 1 malocclusion, class II skeletal pattern, had never undergone orthodontic treatment and had medical records accompanied by a lateral cephalometric radiograph. Through careful selection, as many as 32 lateral cephalometric radiographs were obtained from patients who had class II division 1 malocclusion (figures 1 and 2).
Figure 1 (left) and 2 (right).
Lateral cephalometric radiographs of patients who met the inclusion criteria were used in this study to undergo respiratory tract analysis according to the McNamara method (left). The relation of the dentition of the patients involved in this study shows an incisive relation that is typical of class II division 1 malocclusion where there is a marked increase in overjet and overbite.
In 1993, McNamara evaluated the upper respiratory tract with a radiographic projection technique of lateral cephalometry and anteroposterior.7 In this case, analysis with lateral cephalometric radiographs was performed to see whether there was a deviation of the upper respiratory tract in the nasopharynx caused by adenoid and oropharyngeal hypertrophy due to tonsillar hypertrophy. While analysis with anteroposterior cephalometry was performed to see irregularities in the upper respiratory tract in the nasal region.8
Pharynx has a length of about 12-14 cm, shape like tubes and consist of membrane and muscular tissue. Pharynx or pharyngeal airway is divided into nasopharynx, oropharynx and laryngopharynx or hypopharynx and is located posterior oro-nasal and larynx. It starts from the cranium base and ends at the sixth cervical vertebra where at the lower border there is a cricoid cartilage.9,10 The nasopharynx forms the upper part of the respiratory system, located behind the nasal cavity and above the soft palate. In the anterior part, the nasopharynx is connected to the nasal cavity while the posterior part extends downward as the oropharynx. The main function of the nasopharynx is to facilitate respiration and swallowing during normal physiological processes.
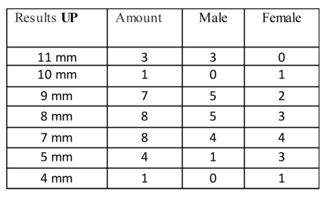
Airway analysis introduced by McNamara and used in this study. It was conducted on all samples, namely 32 lateral cephalometric radiographs. This analysis is divided into two measurements, namely for the upper pharynx (UP) and lower pharynx (LP). Through these two measurements an illustration of the presence of a disturbance in the respiratory tract can be obtained.11 For this measurement, the entire lateral cephalometric radiograph is traced includes the measurement area for the upper pharynx and lower pharynx (figure 3).12
Figure 3. Airway analysis is carried out on all lateral cephalometric radiographs collected to measure upper pharynx (UP) and lower pharynx (LP) according to McNamara method.
After tracing, upper pharynx and lower pharynx measurements are performed. The upper pharynx is measured from one point on the posterior border of the soft palate to the closest point on the pharyngeal wall. Measurements are taken in the anterior half of the soft palate because the area adjacent to the posterior opening of the nose is very important in maintaining a patent upper respiratory tract. Respiratory obstruction is determined when the measurement produces a distance of 5 mm or smaller. The average normal size is 15 to 20 mm. For the lower pharynx, measurements are made on the lower pharynx width which is the distance at the junction of the posterior border of the tongue and the inferior border in the mandibular part to the closest point on the posterior pharyngeal wall. The average size is normally 11 to 14 mm. A smaller than normal lower pharynx value indicates a disorder that may be caused by the position of the tongue more posteriorly.
RESULTS
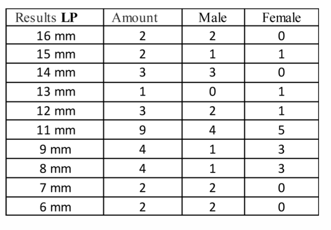
Upper and lower pharynx measurements performed on 32 lateral cephalometric radiographs gave the following results: 32 collected radiographs consisted of 18 male patient radiographs and 14 female patient radiographs. The results of measurements carried out at the upper pharyngeal showed that all patients had obstruction (less than 11 mm). Variations in measurement results can be seen in table 1.
Table 1. Variation in the results of the upper pharynx measurement
The measurement results in the lower pharyngeal showed a slight difference, ie 20 patients indicated normal conditions and only 12 patients indicated obstruction with a yield of 9mm and smaller.
Table2. Variations in measurement results of lower pharynx
Signs of obstruction obtained in the measurement of the lower pharynx are evenly divided, ie, 6 in both male and female patients. However, the measurement results are smaller, namely 7 mm and 6 mm only obtained from male patients, each of 2 persons.
DISCUSSION
The results of this study clearly show a close relationship between the obstruction of the upper respiratory tract with Class II division 1 Angle malocclusion in patients who come to the dental clinic of the Faculty of Dentistry, Prof.DR. Moestopo University. However, more male patients who showed upper respiratory tract obstruction in the study could not be generalized because the number of male patients participating in this study was indeed more than female patients.
Class II division 1 Malocclusion is a malrelation which is much influenced by disturbances in the growth and development of the jaw bone, especially the mandible which is more retrusive than the upper facial bone structure. This malrelation is also associated with functional disorders or abnormalities in the upper respiratory tract as well as the temporomandibular joints.13,14
Muto et al. (2008) showed that craniofacial abnormalities such as retrusive mandible, with a short body of the mandible accompanied by a backward and downward pattern of rotation can cause reduced size of the pharyngeal respiratory tract. The size of pharyngeal space is determined primarily by the relative growth and size of the soft tissues surrounding the dentofacial skeleton.15 There is a significant relationship between pharyngeal dimensions and craniofacial abnormalities.16 Memon et al. in their study found that several skeletal characteristic such as retrusion of the maxilla and mandible and vertical maxillary excess in hyperdivergent patient may lead to narrower anteroposterior dimensions of the respiratory tract.17 Other scientists have come to the conclusion that class II division 1 malocclusion is associated with a narrower upper airway structure without retrognathia.18 This narrower upper airway structure which also indicates that there might be an obstruction in upper respiratory tract can be caused by several things including congenital abnormalities, adenoid hypertrophy, tonsillar hypertrophy, retrusive mandible and obesity. Moving on from this thought, early detection efforts will be very important in preventing the occurrence of class II division 1 malocclusion which in the implementation can be either in the form of preventive or interceptive orthodontic treatment. As stated by Ceylan et al. In their study, pharyngeal dimensions of various sagittal and vertical facial types can help an orthodontist in various ways – especially during orthodontic diagnosis and treatment planning.19 In the previous studies it was found, that the pharyngeal structures continue to grow rapidly until 13 years of age. In this study, the age of patients ranged from 8 years to 11 years. This means that the pharyngeal dimension still has the opportunity to grow and develop. If at this early age, pharyngeal dimension reduction can be detected related to the condition of malocclusions and immediate interceptive orthodontic treatment is carried out, especially with the opportunity to make corrections to skeletal patterns given the patient's age of growth, so that a good skeletal pattern is expected to affect growth and good development of the pharyngeal dimension. Comprehensive corrections like this are expected to provide more valuable benefits to the patient itself. Collaboration with doctors on ear, nose and throat specialist should be seriously considered to maximize the results obtained.
CONCLUSION
All patients with Class II division 1 malocclusion in the study were experienced upper respiratory tract obstruction. This fact indicates that the dentist has an important role to detect the presence of obstruction or disturbance in the tract that may affect the incidence of class II division 1 malocclusion. Thus, efforts to do preventive or interceptive orthodontics can be optimized if the detection of this condition can be done early so that more beneficial for the patient in terms of aesthetics of facial appearance and patient profile. Statement of conflict of interest
The authors declare no conflict of interest
Anggara et al.,Evaluation of respiratory tract in angle class ii division 1 malocclusion of deuteromalay sub-race patients in faculty of dentistry, university prof.dr.moestopo.2018:4(2);31-36
Subscribe now for latest articles, news.