

Journal of Multidisciplinary Dental Research
Volume: 4, Issue: 2, Pages: 13-24
Original Article
Princy Anna Mathew1, Radhika2, Amit Walvekar3, B.S. Jagadish Pai4, Arun Varghese5
1Final Year Student, Department of Periodontics and Implantology, Coorg Institute of Dental Sciences, Karnataka, India.
2Reader, Department of Periodontics and Implantology, Coorg Institute of Dental Sciences, Karnataka, India.
3Professor & HOD, Department of Periodontics and Implantology, Coorg Institute of Dental Sciences, Karnataka, India.
4Former Professor &HOD, Department of Periodontics and Implantology, Coorg Institute of Dental Sciences, Karnataka, India.
5Senior Lecturer, Dept. of Periodontics, Indira Gandhi Institute of Dental Science, Pondicherry.
Corresponding
Princy Anna Mathew
Final Year MDS,Coorg Institute of Dental Sciences, Karnataka, India
Ph : +918296456788
e-mail:[email protected]
Received Date:15 September 2018, Accepted Date:20 September 2018, Published Date:25 September 2018
Background and Objective: Periodontitis and diabetes have a combined systemic and local effect on tooth supporting structure and has been reported for decades. The gold standard treatment protocol would be SRP, which when combined with Low level laser therapy has an additional benefit in the reduction of clinical parameters and HBA1c levels. This study reveals the effect of LLLT as an adjunct to conventional SRP in the HBA1c levels in blood in patients with type 2 DM with Chronic periodontitis.
Materials and Methods: Study group consists of two groups, Group A (control) and Group B(test) each comprising of 15 subjects. Group A were treated with SRP followed by irrigation with normal saline and Group B were treated with SRP and LLLT followed by OHI reinforced on 1 , 7 and 30 day of visit for both groups.
Results: Group A and Group B showed statistically significant results from baseline to 3 months and from baseline to 6 months but no statistically significant result was there from 3 months to 6 months. Intergroup comparison between Group A and Group B showed a greater reduction in clinical parameters and HBA1c levels in Group B than Group A.
Conclusion: LLLT along with SRP shows a significant reduction in clinical parameters and HBA1c levels in type 2 DM patients. Even though there is significant reduction from baseline to 3 months and 6 months, there is no effect from 3 months to 6 months. This depends on the recolonization and the short-term benefits of LLLT. To conclude, LLLT along with SRP gives a reduction in clinical parameters and HBA1c levels in patients with type 2 DM with chronic periodontitis.
Keywords:Chronic periodontitis, Diabetes mellitus, Low level laser therapy, Glycosylated Hemoglobin.
Periodontitis is considered as the 6th complication of diabetes, which has an established destruction of tooth supporting structure by multifactorial disease progression. There is an established inter-relationship between diabetes and periodontitis. Current study suggested that both diabetes and periodontitis have a relatively high incidence in general population (diabetes 16% and periodontitis 14%) and these studies tend to support the higher incidence and severity of periodontitis in patients with DM.
Recently studies indicate accurate blood glucose level has been diagnosed by glycosylated hemoglobin assay (HBA1c). Glycosylated Hemoglobin assay measures the amount of glucose irreversibly bound to the hemoglobin molecule. Thus, this assay is of great significance to the periodontist in monitoring long term control of blood glucose levels.
Scaling and root planing has been the signature periodontal therapy by which most of the periodontal conditions can be effectively managed. Several studies have reported that effective management of periodontitis with SRP provides a dual benefit for diabetic patients. Miller and Grossi stated that successful treatment of periodontal infection is associated with better glycemic control1,2.
Laser therapy has been used in clinical periodontics aiming at reducing bacteria to stimulate regeneration of tissue and for its anti- inflammatory effect. Diode Laser used as an adjunct to periodontal therapy significantly reduces gingival inflammation compared to SRP alone in DM2 patients3.
This study aims to compare and evaluate the effect of low-level laser therapy as an adjunct to scaling and root planing (SRP) and glycosylated hemoglobin (HbA1c) levels in blood in patients with type 2 diabetes and chronic generalized periodontitis.
MATERIALS AND METHODS
Study patient were randomly selected from the outpatients attending the Department of Periodontics and Implantology, Coorg Institute of Dental Sciences, Virajpet during the period February 2017 - May 2018. Study was conducted following clearance from Institutional Review Board (IRB) of Coorg Institute of Dental Sciences. (Reference Number: IRB/CIDS/53/2016 received on 14/11/2016.) A special proforma was used consisting of a brief case history, clinical examination and recordings of clinical parameters at baseline, 3 months and at the end of 6 months. Oral hygiene instructions for supragingival plaque control were given and written consent was obtained from the patient.
Study group consist of two groups, group A (control) and group B(test) consisting of 15 subjects each. Group A treated with SRP followed by irrigation with normal saline and Group B sttreated with SRP and LLLT. OHI reinforced on 1th, 7th, and 30thday of visit for both the groups.
INCLUSION AND EXCLUSION CRITERIA
Patients 30 years or more with chronic periodontitis having probing pocket depth ≥ 5mm, having minimum of 20 or more teeth, diagnosed with type 2 diabetes of more than 3 months duration and currently under the care of a physician for diabetes management with no change in diabetes related medications during 3 months prior to enrolment with screening HbA1c values within the range of 6% to 7% and no prior periodontal therapy were included in the study while patients suffering from any known systemic disease other than diabetes like renal disorders, anemia, hyperthyroidism, etc., patients who had a physician visit within the last 30 days because of hyperglycemia or diabetes related complications, chronic or continuous use of non-steroidal antiinflammatory drugs within the preceding two months, patients under systemic antibiotics, corticosteroids or immunosuppressive drugs, pregnant women or lactating women were excluded from the study. Subjects who are smokers, tobacco or alcohol users were also excluded.
CLINICAL PARAMETERS
Clinical measurements were such as Plaque Index (PI) (Silness and Loe,1964), Gingival Index (GI) (Loe H and Silness J), Modified Sulcular Bleeding Index (Mombelli, 1987), Probing Pocket depth (PPD), Clinical Attachment Loss (CAL) were made using calibrated manual probe (UNC – 15 probe) in 6 sites per tooth and rounded off to the nearest mm. Clinical parameters were recorded at baseline, 3rdmonth and 6thmonth respectively. Customized acrylic stents were used to standardize the measurements of the clinical parameters.
SAMPLE COLLECTION (HBA1c)
10 ml of venous blood sample was collected before the periodontal examination and was analysed by a single laboratory technician. Venous blood sample was added to EDTA using aseptic techniques.
SURGICAL PROCEDURE
Patients were randomly selected by flip of a coin into group A and group B. Group A received SRP and saline irrigation and Group B received SRP and LLLT with 810nm Picasso diode laser. A continuous mode (CW) was used at non-contact mode along the tissues with the 300µ diameter laser delivery tip at a constant speed of 1mm/sec. The tip was positioned externally at the base of the pocket according to the PPD, lingually and buccally in a non-contact mode, at a 900 angle to the long axis of the tooth, in a sweeping motion all over the area, starting apically and moving upwards to the top of the pocket. 0.1w power per site for 60 sec was delivered4. Three laser sessions at an interval of 30 seconds were given on the first appointment (baseline), followed by two sessions on the 7th day and then one session on the 30th day (a total of six sessions for each site). Patients were reevaluated after 3 months and 6 months for assessing their periodontal status and Blood samples were collected for the assessment of Glycosylated Hemoglobin level.
STATISTICAL ANALYSIS
Pearson chi-square test and independent T test were used to analyse baseline and periodontal parameters and Mann-whitney u test for intergroup comparison.
RESULTS
The present study was aimed to evaluate whether nonsurgical periodontal treatment with and without low level laser therapy improves clinical parameters and metabolic (HBA1c) values in chronic periodontitis patients with type 2 diabetes mellitus. There were no complaints such as discomfort, sensitivity or pain from subjects immediately after laser biostimulation as well as 6 months post-therapy.A total of 30 subjects were divided into two groups of 15 each. Each patient underwent a series of 5 appointments and were followed up for a period of 6 months. The treatment protocol is summarized in Table 1.
Table 1: Study Design
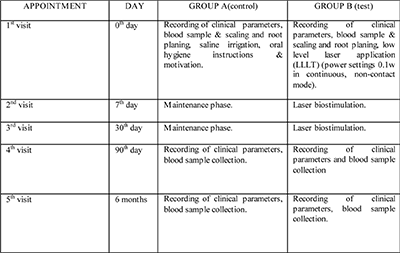
The baseline demographic data of the participants are provided per study group in Table 2 and Table 3 shows the baseline comparison of periodontal parameters and HbA1C levels in between the control and test groups analyzed by Independent t Test.
Table 2: Baseline demographic data of the study patients.
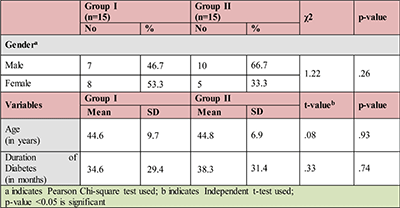
At baseline, no statistically significant differences in clinical parameters are found among the treatment groups except for CAL values (p-value = 0.002) [Table 3]. Whole-mouth clinical parameters showed statistically significant reduction at all time points after treatment compared with baseline in both groups. (p-value < 0.05). However, there is no statistically significant difference in PI and GI between the groups at any time points (p > 0.05). A statistically significant difference is seen in the values of BOP, PPD and CAL. The mean BOP values between the groups differed significantly at 6th month. (p-value = 0.01), The mean PPD values between the groups showed statistical significance at both 3rd and 6th month respectively. (p-value < 0.001). The mean CAL values between the groups showed statistical significance at both 3rd and 6th month respectively. (p-value < 0.001).
The mean and standard deviation of PI in Group I (control) is 2.54 ± 0.81mm; 1.35 ± 0.57mm and 1.26 ± 0.62mm at baseline, 3rd and 6th post-operative respectively. the mean difference is 1.28. This difference is statistically significant with p-value < 0.001. Though this reduction is not significant from 3rd and 6th post-operative, in Group II (test), the mean and standard deviation at baseline is 2.08 ± 0.64mm which reduced to 1.06 ± 0.65mm and 1.13 ± 0.94mm at 3rd and 6th month post-operative. The mean difference is 1.02 and rd th0.95 between baseline-3rdmonth and baseline-6th month. This difference is statistically significant with p-value < 0.001. But the reduction is not significant from 3rd and 6th post-operative.
The mean and standard deviation of GI in Group I (control) is 2.17 ± 0.46mm; 1.18 ± 0.57mm and 1.28 ± 0.49mm at baseline, 3rd and 6th post-operative respectively. When compared between baseline and 3rdmonth post-operative, the mean difference is 0.99 and between baseline and 6thmonth, the mean difference is 0.89. This difference is statistically significant with p-value < rd0.001. The GI values have reduced in the 3rdmonth as compared to baseline, but have elevated by the 6thmonth, though it is not statistically significant, in Group II (test), the mean and standard deviation at baseline is 1.76 ± 0.62mm which reduced to 1.00 rd th± 0.72mm and 1.12 ± 0.65mm at 3rd and 6th month post-operative. The mean difference is 0.76 and rd th0.64 between baseline-3rd month and baseline-6th month. This difference is statistically significant with p-value < 0.001 and p-value = 0.005 respectively . The GI values have reduced in the 3rd month as compared to baseline, but have elevated by the 6th month, though it is not statistically significant.
The mean and standard deviation of BOP in Group I (control) is 1.43 ± 0.42%; 0.652 ± 0.31% and 0.990 ± 0.12% at baseline, 3rd and 6th month post-operative respectively. When compared between baseline and 3rd month post-operative, the mean difference is 0.778, between baseline and 6thmonth, the mean difference is 0.44 and between 3rd and 6th months it is 0.338. This difference is statistically significant with p-value < 0.001. The BOP values reduced from baseline to 3rd month but then elevated in the 6th month post-operative and it is statistically significant with p-value < 0.001. Similarly in Group II (test), the mean and standard deviation at baseline is 1.37 ± 0.40% which reduced to 0.510 ± 0.27% and 0.818 ± 0.20% at 3rd and 6th month post-operative. The mean difference is 0.86 and 0.552 between baseline-3rd month and baseline-6th month. This difference is statistically significant with p-value < 0.001. The BOP values reduced in the 3rd month as compared to baseline, but have elevated by the 6th month post-operative and it is statistically significant with p-value < 0.001.
The mean and standard deviation of PPD in Group I (control) is 4.25 ± 0.12mm; 1.78 ± 0.21mm and rd th2.10 ± 0.42mm at baseline, 3rd month and 6th month post-operative respectively. When compared between baseline and 3rd month post-operative the mean difference is 2.47; between baseline and 6th month the mean difference is 2.15 and between 3rd and 6th months it is 0.32. This difference is statistically significant with p-value < 0.001 at baseline and 3rd month and baseline and 6th month hand p-value = 0.023 at the 3rd month and 6th month postoperative, in Group II (test), the mean and standard deviation at baseline is 4.22 ± 0.13mm which reduced to 0.915 ± 0.41mm and elevated to 1.31 ± 0.02mm at 3rd month and 6th month post-operative. The mean difference is 3.305 and 2.91 between baseline and 3rd month and baseline and 6th month. This difference is statistically significant with p-value < 0.001. The PPD values reduced in the 3rd month as compared to baseline, but have elevated by the 6th month post-operative and it is statistically significant with p-value = 0.002.
The mean and standard deviation of CAL in Group I (control) is 4.90 ± 0.09mm; 1.35 ± 0.34mm and rd th1.69 ± 0.47mm at baseline, 3rd month and 6th month post-operative respectively. When compared between baseline and 3rd month post-operative the mean difference is 3.55, between baseline and 6thmonth the mean difference is 3.21 and between 3rd and 6thmonths it is 0.34. This difference is statistically significant with p-value < 0.001 at baseline and 3rd month and baseline and 6th month and p-value = 0.013 at 3rd and 6th month respectively, in Group II (test), the mean and standard deviation at baseline is 4.76 ± 0.13mm which reduced to 0.778 ± 0.34mm and 1.29 ± 0.07mm at 3rd and 6th month post-operative. The mean difference is 3.982 and 3.47 between baseline - 3rdmonth and baseline - 6th month. This difference is statistically significant with p-value < 0.001. The CAL values reduced in the 3rd month as compared to baseline, but have elevated by the 6th month post-operative and it is statistically significant with p-value < 0.001.
Baseline comparison of HbA1c levels for Group I and Group II which are 6.62 ± 0.31gm%, 6.61 ± 0.32gm% achieved by Independent t test. the mean and median HbA1c levels of Group I. The mean HbA1c level of control group is reduced from 6.62 ± 0.31gm% at baseline to 6.46 ± 0.28gm% at the rd3 month and further reduced to 6.26 ± 0.30gm% that the 6 month which are statistically significant with p-value < 0.001 and 0.002.
Control group showed a 2.4% and 3.1% reduction with respect to baseline at 3rd and 6th month respectively, the mean and median HbA1c levels of Group II. The mean HbA1c level of test group was reduced from 6.61 ± 0.32gm% at baseline to 6.23 ± 0.26gm% at the 3rd month and further reduced to 6.06 ± 0.23gm% at the 6th month which are statistically significant with p-value = 0.009, p-value < 0.001 and p-value < 0.001 respectively. Test group showed a 5.7% and 2.7% reduction with respect to baseline at 3rd and 6th month respectively.
DISCUSSION
Periodontitis and diabetes mellitus are common chronic diseases worldwide. There is substantial evidence to support that periodontal disease could lead to poor metabolic control in diabetic individuals and also diabetes in turn acts as a risk factor for periodontal disease. Hyperglycemia results in low insulin level production which in turn induce inflammation and impede wound healing; this could explain why individuals with periodontitis have high HbA1c levels.
Laser therapy has been used in clinical periodontics aiming at reducing bacteria to stimulate regeneration of tissue, and for its anti- inflammatory effect. Because of the lower energy densities and wavelengths used in LLLT, many therapeutic effects of the low-power laser have been claimed which included acceleration of wound healing,enhanced remodeling and repair of bone, restoration of neural function after injuries and reduction of pain.5-8 It is able to easily penetrate into the tissues, resulting in biomodulation effects on cells and tissues. The practical use of LLLT is easy once the optimal dose and target points have been determined.
The classical parameters for diagnosis of periodontitis are clinical parameters such as probing depths of the gingival crevice, bleeding on probing, clinical attachment levels and radiographic analysis.9 These parameters are reliable to assess the severity of periodontitis under the condition of significant tissue destruction. However, measuring these parameters has poor prognostic impact and therefore oral fluids have been investigated as an alternative diagnostic and prognostic approach.10-11
HbA1c is one type of diagnostic tool, used primarily to assess control of blood glucose over prolonged periods of time in diabetic patients. A total of 30-35% of reduction in microvascular complications and 14-16% macrovascular complications occurs per 1% absolute reduction in glycated hemoglobin. It is a reflection of the mean blood glucose concentration over the preceeding 1-3 months, while fasting blood sugar and random blood sugar reflects differences over a short period of time, which is clinically less relevant. This study assessed the effect of low-level laser therapy as an adjunct to scaling and root planing (SRP) on HbA1c levels in blood in patients with type 2 diabetes and chronic generalized periodontitis.
Control group has been used in the present study in order to estimate the additional effects of LLLT as an adjunct to SRP in patients with diabetes mellitus. The periodontal parameters measured in our study included PI, GI, BOP, PPD and CAL and were correlated with HbA1c levels. Low level lasers have been used for experimental and clinical studies on bone repair. The 830 nm wavelength is known to be a fair tissue penetration laser, because hemoglobin and water have a low level of absorption for this wavelength.12 The application of this unit was advantageous as it is a small, easy to use and fairly inexpensive device.
DM2 patients showed significant improvements in all clinical periodontal parameters except for PI and GI values at 3rd and 6th months postoperatively after SRP as well as SRP+LLLT treatments compared to baseline. Also, SRP+LLLT group showed comparatively superior results at all time phases. The reduction in plaque scores over a period of 3 months and 6 months in the test group when compared with control group was in agreement with the study by Almeida et al, 2006 and Grossi et al.2,1997, who reported significant decrease in plaque scores from baseline to 3 months, 3 to 6 months and from baseline to 6 months respectively13 . The percentage decrease of PI of the test group (49.1%) has been found to be higher than that of the control group (46.8%), after 3 months, which was in agreement with the findings by Qadri et al. and Makhlouf et al.14,4
Gingival Index System was introduced for the assessment of the gingival condition and records qualitative changes in the gingiva. GI does not consider periodontal pocket depth, degrees of bone loss or any quantitative change of periodontium.15 This criteria is entirely confined to qualitative changes in the gingival soft tissue. In our study intragroup comparison shows significant reduction from baseline to 3 months and baseline to 6 months but intergroup comparison shows no significant reduction. There is 45.6% and 43.2% decrease in control and test groups from baseline to 3 months postoperatively. Reduction in GI values is due to removal of local stimulating factors and reduction of the severity of inflammation and this is in accordance with the study conducted by Qadri et al.14
Increased PPD and loss of clinical attachment are pathognomic for periodontitis and hence, pocket probing is a crucial and mandatory procedure in diagnosing periodontitis and evaluating the success of periodontal therapy. PPD is still the most important clinical parameter for periodontal diagnosis (Lang and Bragger).16 In our study there is significant reduction of PPD values from baseline to 3rdmonth and baseline to 6th month in both the groups. This is in agreement with another study by Novokovic et al. which shows that meticulous SRP has eliminated the bacterial burden which resulted in a marked reduction in inflammation. Complete re-epithelialization and healing by long junctional epithelium might have resulted in reduction of PPD and gain in CAL.17 A study by Moritz et al,1998 found significant reduction in PPD values in the laser treated (DL) sites than sites treated with SRP alone.18 When the results of changes in PPD were compared for the two groups in the present study, the effect of laser is found to be statistically significantly higher in reducing PPD values after 3 months. Moreover, the percentage improvement of PPD with respect to time in the laser group (78.3% vs 58.1%) is significantly higher at the periods from baseline to 3 months than that of the control group. These results are in accordance with those of Qadri et al. and Makhlouf et al. respectively.14,4
Significant reduction in BOP and CAL are also evident in our study at the 3rd month as compared to 6th month in the test group treated with LLLT. There is a reduction of 83.7% in CAL in the test group at 3 months as compared to 72.4% in the control group. There is statistically significant rise in BOP and PPD values at the 6th month in both the groups. These findings reveal that the adjunctive use of LLLT has promising effects at the 3rd month. Our results for CAL values are in agreement with those obtained by Saglam et al.2014; Ustun et al. 2014; Dukic et al. 2013; Kreisler et al. 2005; Qadri et al. 2005 and Moritz et al. 1998.19-22,14,18 A recently published meta-analysis by Slot et al. 2014, indicated that adjunctive use of the DL with SRP provided significant improvements only in GI and bleeding scores compared to SRP alone and it was concluded that the evidence considering the adjunctive use of DL is judged to be moderate for changes in PD and CAL.23 Kreisler et al. in 2005 found a greater reduction in probing depth and increase of attachment gain with the adjunctive application of laser compared to SRP alone.22 Contrary to our findings , some researchers suggested that DL did not provide any additional clinical benefits when compared with conventional treatment. These controversial reports might be the result of different wavelengths, application power densities, type of laser fiber and application time.
The major finding in the present study is that in both the groups, the percentage of HbA1c is reduced. There has been 2.4% decrease from baseline to 3rd month and 3.1% decrease from 3rd month to 6th month in Group I, which is in accordance to the study conducted by Telgi et al. rd(0.58%). 5.7% decrease from baseline to 3rd month and 2.7% decrease from 3rd month to 6th month in Group II shows the short-term effect of LLLT which has also been observed in a study conducted by Makhlouf et al, 2012.4 The former result is consistent with various studies reported by West Felt et al. and Kiran et al.which suggested that there was a marked improvement in both periodontal parameters and glycemic control in individuals with type 2 diabetes mellitus following periodontal therapy.24-25 They observed the change after 3 months, administered with no changes in medical therapy or diet in DM2 patients with periodontitis. In our study, there is reduction of HbA1c values among both the groups at 3month and 6-month follow-up, with significant acute reduction in the third month and marginal significant reduction in the sixth month. It is in contrast to the study by Christgau et al. who observed no significant change in glycated hemoglobin levels 4-months following non surgical therapy.26 However, the study group consisted of only 3 individuals and the median glycated hemoglobin level was only 6.5% at baseline, whereas in the present study, the mean HbA1c at baseline was 6.6%.
The intragroup comparison of mean HbA1c showed statistically significant reduction in both test and control groups. These findings suggest that both SRP and SRP along with LLLT has some additional effects on the glycaemic control. It has also been observed that SRP along with LLLT treatment provided better reductions in HbA1c levels as compared to SRP treatment alone. Intergroup comparison suggests significant reduction in the HbA1c values in the 3rd month in both groups which is in accordance with the results obtained by Kocak et al, 2016.27 The lack of any additional benefits from the use of LLLT on diabetic patients in the 6th month suggests the short-term effect of laser, which might be due to the low power used or due to the mode that was used (non-contact). The minimum number of sessions to obtain a positive effect of LLLT is still not known. Makhlouf et al. used 10 sessions equal to that of Pejcic et al., although in the latter study it was treated daily.4,28 Qadri et al. used one session per week during 6 weeks and Aykol et al. used only 3 sessions, concentrated to the first week after SRP14,29. In our study the schedule for laser treatment was 3 sessions on the day of SRP, 2 sessions on the 7th day and 1 session on the 30th day respectively. According to Pinheiro and Gerbi, 2006, LLLT is most effective if the treatment is administered at early stages when high cellular proliferation occurs.30
Our study is the first of its kind to suggest the effects of LLLT in HbA1c and clinical parameters in type 2 DM patients with chronic generalized periodontitis. The reduction of HbA1c levels by periodontal therapy in type 2 DM patients with periodontitis has been reported by Grossi et al.2 Kiran et al.suggested that the improvement in the HbA1c values was possibly due to the reduction in the GI and BOP values.25 In contrast to our study design, Kiran et al.25 had the criteria of HbA1c level between 6% and 8%. In addition to the suggestion of Ryan et al.we speculate that many factors influence the short-term glucose level of a diabetic patient and that one of these factors is medical care.
There are certain limitations in our study which include a smaller sample size and fewer sessions of laser therapy. Moreover, other factors such as BMI, obesity, different medications taken by the patients during the course of the study, different diet and lifestyles among the subjects, which might play a role in the elevation or depression of periodontal findings has not been included in our study. Further long-term studies to standardize the dose and application of laser therapy as an adjunct to SRP in type 2 DM patients with periodontitis should be encouraged, so as to avoid surgical interventions in such patients.
CONCLUSION
Within the limitations of the present study, the following conclusions may be derived:
The positive outcome of the therapy is very promising and it may be eventually implemented in the daily practice for the treatment of periodontal inflammatory diseases in combination with conventional therapies. Also, oral and periodontal health should be promoted as integral components of diabetes management.
Subscribe now for latest articles, news.