Journal of Multidisciplinary Dental Research
DOI: 10.38138/JMDR/v5i2.8
Volume: 5, Issue: 2, Pages: 92-98
Case Report
Srirangarajan Sridharan1, Aparna Satyanarayan2, Veena Malgi3, Ramya Raghu4, Ashish Shetty5, Chinmaya Kumar Samantaroy6
1MDS, Professor, Department of Periodontics. E-mail: [email protected]
2MDS, Reader, Department of Periodontics. E-mail: [email protected]
3MDS, Post graduate student, Department of Periodontics. E-mail: [email protected]
4MDS, Professor and Head, Department of Conservative and Endodontics. E-mail: [email protected]
5MDS, Professor, Department of Conservative and Endodontics. E-mail: [email protected]
6MDS, Post graduate student, Department of Conservative and Endodontics. E-mail: [email protected]
Corresponding Author:
Dr. Srirangarajan Sridharan
Department of Periodontics, Bangalore Institute of Dental Sciences and Postgraduate Research Centre, 5/3, Hosur Road, Bangalore - 560029.
Tel: 91 9844292297
Email ID: [email protected]
Fax: 080-41506025
Received Date:10 December 2019, Accepted Date:15 December 2019, Published Date:31 December 2019
Introduction: Furcal perforations compromise the health of the periradicular tissues and threaten the viability of the tooth. Perforation repair is a very attractive and frequently successful alternative to extraction of the involved tooth. Diagnosis and repair of furcal perforation, abscess have remained a diagnostic and therapeutic dilemma for the clinician. We believe this case report is the first of its kind to compare the repair of furcal perforation due to iatrogenic causes with mineral trioxide aggregate (MTA) and bone graft by conventional surgical technique and laser assisted periodontal therapy in mandibular molars.
Case presentation: Two patients presenting with clinical presentation and diagnosis of furcal abscess due to iatrogenic causes were treated and followed up for six months. The furca were exposed surgically. The furcation area in one patient was debrided by conventional periodontal therapy while in the other laser assisted periodontal therapy was instigated using diode laser, and the perforation sealed with mineral trioxide, bone graft was placed in the interradicular area. Clinical and radiographic examinations were conducted at base line and 6 months.
Conclusion: During the 6 month follow up satisfactory resolution of the clinical and radiographic defect in the interradicular region was achieved by both conventional surgical and laser assisted periodontal therapy.
Keywords: furcal abscess, perforation repair, mineral trioxide, diode laser, bonegraft
Furcal perforation is a detrimental complication that can occur during preparation of endodontic access cavities or exploring canal orifice of multirooted teeth.1 Coronal flaring instruments have sensitized the dentine between the roof of the furca and canal orifice to fracture, thus giving way to a communication between the two. The result is a chronic inflammatory reaction of the periodontium (characterized by the formation of granulation tissue) that can lead to irreversible loss of attachment or loss of the tooth. Such perforations are managed surgically or nonsurgically, depending upon the characteristics of the case.2 Prognosis may be questionable if treatment involves a lesion occurring at the level of the radicular furcation, but is usually good if diagnosed correctly and treated with a material that is biocompatible and can adequately seal the perforation.3
A study group in Toronto found that in retreatment cases two factors affected the success rate of the treatment significantly: (a) the presence of a preoperative radiolucency and (b) the presence of a preoperative perforation4. However, there is a paucity of evidence-based research upon which treatment decisions can be based upon. Traditionally, the presence of radicular perforations has been both difficult to determine and manage; and often these teeth are extracted.5,6 MTA* has been applied with good outcome in root-end surgery, direct pulpal coverage, apexification, radicular resorption and repair of lateral radicular and furcal perforations7. Its suitability for management of the above is attributed to its excellent biocompatibility, low induction of inflammation, solubility, capacity for creating a seal between the pulpal chamber and periodontal tissues and its repair capacity. The last of these features can in turn be credited to the antimicrobial properties and high pH (12.5) of MTA, which promote formation of cementum and bone, which in turn allow regeneration of the periodontal ligament around the site of injury8 The use of diode lasers for soft-tissue healing has been reported by Capon, et al9 Al-Watban, et al10 and Güngörmüs and Akyol11 in animal models as well as in humans by Amorim et al.12 Ciancio et al13 studied the effect of the 810-nm diode laser in conjunction with scaling and root planing on periodontal wound healing and concluded that the diode laser improved the softtissue healing and increased patient comfort.
To our knowledge there has been no previous reports describing the use of MTA with bone graft in furcal perforation with and without laser.
Case presentation 1:
A 52 year old female patient was referred from department of Endodontic to the Department of Periodontics at Bangalore Institute of Dental Sciences and Postgraduate Research Centre in March 2012, for opinion regarding a frequent gingival swelling and dull pain on chewing in relation to mandibular right first molar. A comprehensive medical and dental history revealed that she was systemically healthy. The patient, for the first time, came to the endodontic clinic two years ago in January 2010, with active and at the time, it was diagnosed as pulpal necrosis with acute periradicular periodontitis and root canal therapy was instigated.
The patient was asymptomatic thereafter until December 2011, when she reverted back with a gingival swelling with respect to the same tooth associated with dull pain and exudation. At the time, it was diagnosed as a gingival abscess and the abscess was drained; antibiotics prescribed. (Amoxicillin 500mgs tid x5 days and metronidazole 400mg bid x5days).The abscess recurred for the third time in March 2012 and she was referred to our department for opinion. The tooth was tender on percussion and exhibited no mobility. A localized probing depth of 3mm (mid-buccal) was recorded using University of North Carolina (UNC) 15 periodontal probe# and the horizontal probing depth in the furcation area using Nabers probe# was 7mm. The patient showed no signs of periodontal breakdown in the interproximal areas; after a thorough clinical and radiographic examination a final diagnosis of furcal abscess due to iatrogenic causes was arrived at. (Figure 1a and 1b) Surgical therapy was considered with use of MTA for the furcal communication and bone graft for the interradicular area. Informed consent was obtained and initial phase therapy, comprising oral hygiene instruction, scaling and polishing was carried out; with flap surgery being scheduled after 1 month.

Fig: 1a: Pre operative clinical photograph of case 1 at baseline.
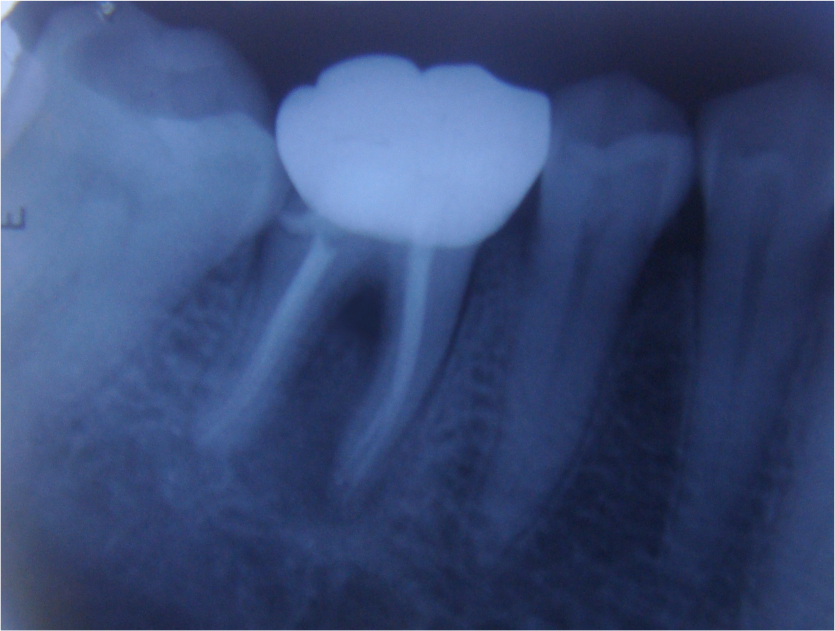
Fig: 1b: Pre operative radiograph of case 1 at baseline
Case management:
A full thickness mucoperiosteal flap was raised with crevicular incision extending from distal surface of mandibular right second premolar to mesial surface of mandibular right second molar; vertical release incisions were given at line angle of the tooth to gain access for debridement. Furcation area was exposed and granulation tissue was debrided using Gracey 5-6, 13-14 and furcation curettes.# The communication in the furca area was sealed with MTA. Interadiculaar area was filled with bone graft (Biograft HA™)¥, collagen membrane (Healiguide™)£ placed and the flap was sutured back.
Post surgical instructions were given and patient was recalled at 1, 3 and 6 month interval post suture removal. (fig 2a and 2b)

Fig: 2a: Post operative clinical photograph of case 1 at the end of 6 months.
Fig: 2b: Post operative radiograph of case 1 at the end of 6 months.
Case presentation 2:
A 21 year old male patient was referred from department of Endodontic to the Department of Periodontics at Bangalore Institute of dental science and post graduate research centre in April 2012, for opinion regarding a recurrent gingival swelling with persistent sinus tract lingually with respect to mandibular right first molar. The patient, for the first time, came to endodontic clinic one year ago in January 2011, with active and at that time, it was diagnosed as irreversible pulpitis with acute apical periodontitis and root canal therapy was instigated. The patient was asymptomatic thereafter for one year (December 2011) at the end of which there was a recurrence of the gingival swelling in the same tooth and a sinus tract opening on the lingual surface. It was diagnosed as a furcal abscess based on clinical and radiographic examination. The abscess was drained, the sinus tract debrided and irrigated with 0.1% povidone iodine. Antibiotics were prescribed (Amoxicillin 500 mgs tidx5 days and metronidazole 400mg bidx5days). The patient responded well and was under maintenance. The patient returned at the end of three months (April 2011) with a recurrence of the swelling, dull localized pain and tenderness on percussion and was treated likewise. There was a recurrence of the same at the end of 1 year (April 2012) when, he was referred to our department. On examination a localized probing depth of 3mm (mid-lingually) was recorded using UNC 15 periodontal probe and the horizontal probing depth in the furcation area using Nabers probe was 8mm. Intra oral periapical radiograph revealed interradicular bone loss. Since the patient showed no signs of periodontal breakdown in the interproximal areas the final diagnosis was given as furcal abscess due to iatrogenic causes and surgical therapy was planned.
Case management:
A full thickness mucoperiosteal flap was raised after crevicular incision in the region extending from distal surface of mandibular right second premolar to mesial surface of mandibular right second molar; vertical release incisions were given at line angle of the tooth to gain access for debridement. Care was given to not exert pressure near the sinus opening area. Furcation area was exposed and before applying the laser, the operating staff and the patients wore special laser-protective glasses. The protocol followed for laser therapy was as follows
Highly reflective instruments or instruments with mirrored surfaces were avoided. Power 2W, continuous mode; in addition the sinus tract was also decontaminated using the same laser (power 3W continuous mode). The communication in the furca area was sealed with MTA, interradicular area was filled with bone graft, collagen membrane placed and the flap was sutured back. Post surgical instruction was given and patient was recalled at 3 and 6 month interval post suture removal (fig 4a and 4b).
Fig: 4a: Post operative clinical photograph of case 2 at the end of 6 months.
Fig: 4b: Post operative radiograph of case 2 at the end of 6 months.
Surgical repair of perforations has received sporadic attention in dental literature and has been supported primarily by case reports or limited studies.14 In this case report we attempted repair of furcal perforation due to iatrogenic factors by conventional and soft tissue laser. As discussed by Weine15 management of perforations demands ‘spontaneity and creative approaches.’ The prognosis of perforations depends on the location, size and time of contamination of the lesion.16 The location of furcal perforations at the level of the epithelial attachment and crestal bone suggest a guarded prognosis.17 Secondly, the size of a perforation represents another important factor in determining the success of the repair procedure. Finally, interval between perforation and repair is one of the critical factors for success.18,19
In our cases patients’ complained of recurrent abscess post endodontic treatment; periodontal breakdown was evident in the furcation region only on radiographs. Surgery was instigated to produce an environment conducive to the regeneration of the periodontium, although complete regeneration would not be possible due to the time lag in initial diagnosis and surgical therapy.20,21,22 Immediate sealing of perforations enhances the repair process due to reduced bacterial contamination of the defect.23
Lateral root perforations sealed with MTA after contamination presented worse repair than the non-contaminated, immediately sealed perforations.24
Amalgam, composite resin and glass ionomer cements have been used for sealing furcal perforation. However, studies have shown that MTA is superior to these materials with respect to marginal adaptation25-28, bacterial leakage28,29 and cytotoxicity30. Main et al concluded that MTA provides an effective seal of root perforations and can be considered a potential repair material enhancing the prognosis of perforated teeth that would otherwise be compromised.
Hence we chose MTA for sealing the perforated site. After debridement of the granulation tissue with either the laser or surgical curettes the furcation area was located, irrigated with sodium hypochloride to decontaminate the area of blood as it could reduce the retention capacity of MTA.31
Success has been reported both with and without the matrix. No matrix was used in either surgery. Both patients were followed up for a period of six months with uneventful healing and the follow up intraoral periapical radiograph showed good repair of interradicular bone in patients. Healing depends on factors mentioned above; it would be erroneous at this juncture to deduce the benefits of laser over conventional surgical debridement. The sinus tract on the lingual side complicates surgeon’s access, flap management and tissue handling during debridement. These hurdles are easily overcome if one uses a laser as it comprehensively decontaminates the sinus tract which otherwise is left alone.
Summary and Conclusion
Conflict of Interest
The authors claim no conflict of interest. No external funding was obtained for the study.
Srirangarajan Sridharan, Aparna Satyanarayan, Veena Malgi, Ramya Raghu, Ashish Shetty, Chinmaya Kumar Samantaroy. Conventional flap versus laser assisted periodontal surgery in the treatment of furcal abscess- a case report. Journal of Multidisciplinary Dental Research. 2019:5(2);92-98
Subscribe now for latest articles, news.